Mental Health Challenges & How to Minimize Them
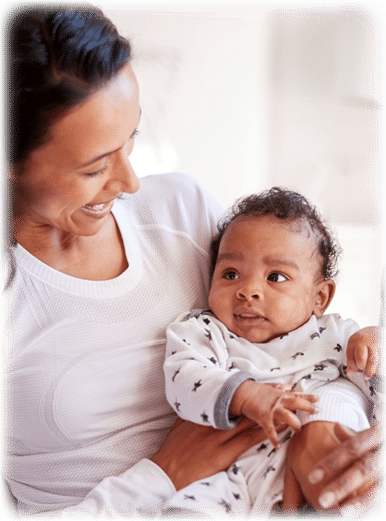
Maternal mental health is so often not acknowledged, maybe misunderstood, and has large impacts (both short and long term), if a mother does not get support. With BirthWorks as a foundation, often many mental challenges that mothers experience are minimized. This is because during childbirth preparation, we help mothers connect to their feelings, process past grief and trauma, and reframe fear about the future. If a mother enjoys the end of pregnancy with the BirthWorks Experience as a foundation, often labor and birth are shorter and easier, because she carries with her more confidence in her own abilities, her body and connection to her baby. Mothers who are content about their birth story eliminates some risk factors that might lead to feeling sad, overwhelmed or self-doubting.
A new mother going home with a newborn, who had a positive labor and birth (or ways to understand and process effectively, if the birth was not her ideal) is empowered by a human-value framework to bring self-compassion and patience, as well as love, to her own experience. She also brings this positive frame to the first moments with her new baby and into newborn care. BirthWorks Philosophy does not guarantee ease in what might be challenging in the transitions - pregnancy to birth to bringing a newborn home - but BirthWorks does empower mothers to pave a path of possibility for health and wellness - for mother and others. Those who experience BirthWorks, often create a loving positive vibe for themselves and from the first moments after birth, and this energy carries into the early hours, then early days and can impact the whole household positively.
Surprises about Maternal Mental Health
Did you know the impact of mental health disorders happens in both pregnancy and in postpartum? Are you aware that it does not matter – about mothers’ race, color, religion (creed), gender, gender expression, age, size, national origin (ancestry), disability, marital status, sexual orientation, or military status – that mental health challenges happen to ALL women. Not feeling well mentally impacts any mother’s ability to care for and bond with their baby, as well as their relationship with their other children and partners. Are you aware postpartum depression can start when the baby is already two weeks old and can last a year? Also, did you know that fathers/partners experience mental health challenges and need support too, and are more likely to be impacted if the mother has mental disorders? What about the idea of loss? - it is connected to emotional experiences of pregnancy and birth (whether that be loss of body/image of self, career, sleep, free time, friends or deeper loss of an infant). About 25% of people experience infant loss at some point - is this well-known? In many cases of mental stress or loss, it is so important to acknowledge the reality, know it is normal at times, that support is needed and with loss there are stages of grief which people handle in their own way and time. It is also key to understand when mental challenges become disorders. Awareness of the context of maternal mental health shifts understanding and opens support for healing.
The System is (mostly) Broken - How to Be Aware of Risk
The system for supporting new mothers is broken in many ways. As much as some mothers do get prenatal care… in many settings often no providers ever ask them - how are you feeling? - and mean it in terms of emotional and mental wellness. Since maternal mental health is a quiet conversation in many systems and cultures, and women want to appear strong and be perceived as good mothers, they are often silent. So, suffering mothers often suffer alone with little or no support. Often women don’t want to burden their partners who go back to work, or their anxiety is just seen as part of good mothering of a newborn, so if signs are there, loved ones might not understand the depth of challenge the mother feels.
Risk Factors for maternal mental disorders include history of mental illness (personal or in their family), past trauma and abuse, exposure to violence (crime, rape or war - or it simply may be worth considering the impact of thoughts that come from exposure to too much violent media), low socio-economic status (and related racial and other trauma), past pregnancy loss (often related to fertility issues or having a past abortion), high-risk pregnancy (traumatic pregnancy or birth, unwanted interventions, cesarean surgery), stress in life, poor social support networks (broken or geographically spread out families, lack of local support), medical/hormonal issues, and even personality that tends toward perfectionism or has high expectations. Keep these factors in mind for those mothers you love, and educate yourself and them with care and compassion.
Maternal Mental Health - The Facts
Most moms experience baby blues in the first weeks after birth due to their hormones returning to normal levels. This may last about six weeks - just the time when the lochia subsides. When moms anticipate this happening, it will ease fears because they will understand it is typical and normal. Symptoms include fatigue, sadness, feeling anxious or overwhelmed, sleep deprived, and worrying about their baby. Anything more extreme should be taken seriously.
Below are the six main maternal health disorders, which impact 15-21% of mothers:
- Depression: impacts 10% pregnant women & 15% postpartum (for up to 12 months) with sadness, fatigue, overwhelm or exhaustion, appetite changes, difficulty with concentration, strong emotions, anxiety, disconnect from baby, maybe consideration of suicide
- Anxiety: impacts 5% pregnant women & 10% postpartum and is underdiagnosed but impacts daily life, as mothers over worry, are edgy, blaming self, find it hard to sleep or eat, are restless, maybe sad
- Panic Disorder: up to 10% of women, builds on symptoms above with extreme anxiety, panic attacks, excessive fear or death, obsession with health, agitation, extreme worry and fear
- Post-Traumatic Stress Disorder (PTSD): impacts 1-6% of women, who most likely had some past difficulty during pregnancy, had an unwanted or unplanned baby (50% of pregnancies in the US for example), experienced medical interventions, inadequate care, serious or perceived threat or injury to self or baby, including sadness, self-esteem dropping, anger, appetite and sleep disturbance, being easily startled, anxiety, avoidance, intense distress from memories, intrusive thoughts, numbness of emotions
- Obsessive-Compulsive Disorder (OCD): impacts 3-5% of women, more than above including intrusive unwanted repetitive thoughts about harm that feel horrifying, tremendous guilt and shame, avoidance, extreme self-doubt, feeling unstable, bizarre thoughts (that may be acted on and hurt their baby) - avoidance behaviors show up, like avoiding tools that could harm (like kitchen knives), not want to change or bathe baby, not eating certain things fearing harm, obsessive checking on the sleeping baby, and need for continual reassurance the baby is fine
- Postpartum Psychosis: impacts 1-2 of 1,000 women, usually in first 2-4 weeks, this is the most severe, with delusions, hallucinations, confusion, mood changes, paranoia, irrationality and acting on irrationalities - so is also the most lethal. (added period)
How to Best Help?
There are tools, methods, treatments, and information available to help new mothers. Just discussion and education about maternal (and parental) burnout and mental health helps make conversation about this more normal. Beyond that, optimally all health professionals should do universal screening for perinatal health disorders. There are early screenings using tools like a Prenatal Risk Screen, Edinburgh Postnatal Depression Scale (EPDS) and Patient Health Questionnaires. Proactively letting mothers know about mental health and wellness is key. Sharing with them that they may be at more risk depending on their history, and providing them holistic and specific treatment options can be very empowering. Just understanding that some of the mental health challenges are normal for most moms decreases self-judgment and makes it easier for moms to see and ask for a break, support and more specific help when needed.
Specifically, for each mother (or family) in need, it is great to help them (starting during pregnancy) to create social support (help with the baby, family and friends visiting, find an interest group (for new moms or other) or a spiritual/faith community, be connected to resources for individual counseling or therapy, and knowing (if needed later) where to find a psychiatric evaluation and medical treatment will help. Also, holistic approaches can make a big difference in overall outlook - such as diet, exercises, yoga and meditation, acupuncture and the use of other healing modalities (massage, breathwork, chiropractic). These give the mother a break, time for self-care and perspective, and help mothers feel like themselves a bit more. Sharing information on mother/baby groups (like those that meet to walk at the park, chat at a coffee shop, at a local library, or to do mom/baby exercise and yoga) can be very helpful. Giving the chance for mothers to get out of the house is so important - as they hear others also feel challenges as new parents and will relax a bit in like-company.
Thank you for reading this and choosing to be part of the awareness that is growing and changing. Together, we can develop positive support for deserving moms – and to transform health outcomes for women in future generations. At BirthWorks, we encourage new parents to take childbirth education preparation classes early in the first trimester - you can find a BirthWorks professional or a virtual immersion course.
* We want to thank Healthy Moms, Healthy Babies in Palm Beach county in Florida. Their May 19, 2002 webinar on this topic. Much of the inspiration to write this and part of the content was inspired by their work and the teaching of the Facilitator Elais Perez at eperez@hmhbpbc.org.